Practice Guide for All-Options Pregnancy Counseling
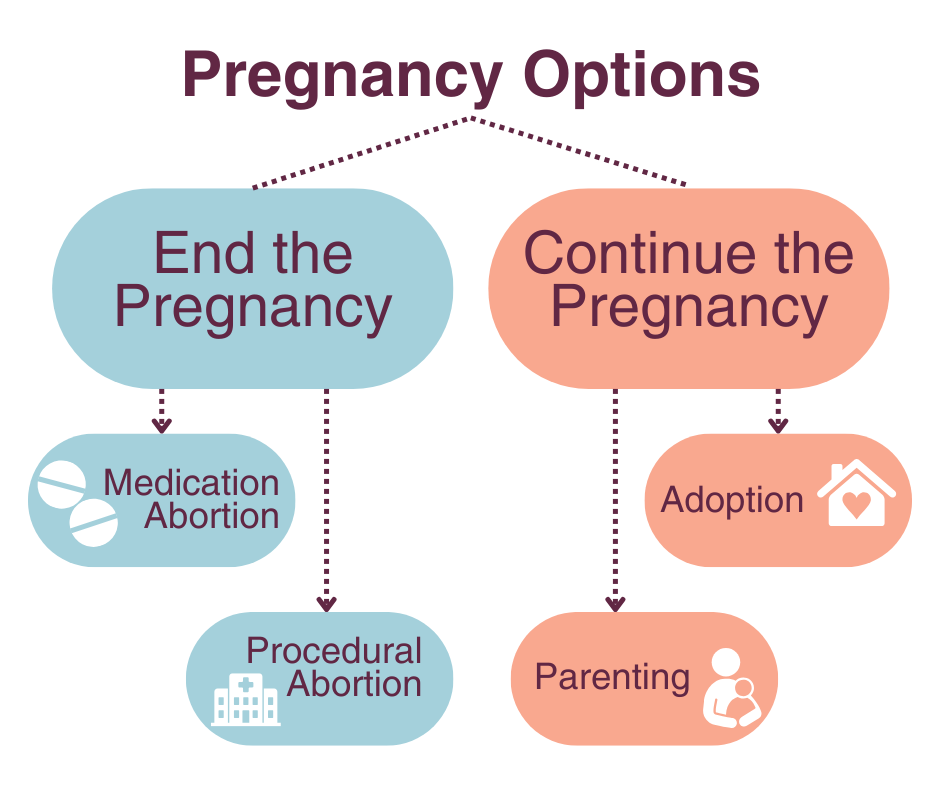
Provide recommends that all pregnant patients be offered information on all pregnancy options, including continuing the pregnancy to parenthood or adoption, or ending the pregnancy with medication or procedural abortion.
Using the recommended methods to counsel patients on all pregnancy options meets patient needs and leads to higher satisfaction regardless of their decision. The following Practice Recommendations were developed by a team of experts and outline the key steps for all-options pregnancy counseling. Click each step to learn more.
Prepare patient for pregnancy test.
- Ensure that the patient agrees to the test and understands how the result will be used.
- Let the patient know you are there to support them whatever the result and whatever decisions they make.
Disclose the pregnancy test result.
- Be clear and use a neutral tone.
- Avoid any judgment or assumption about the patient’s feelings or preferences.
→ “Your pregnancy test came back positive, which means you are pregnant.”
- Avoid any judgment or assumption about the patient’s feelings or preferences.
- Pause for patient response.
- Allow some time for the patient to absorb the information.
- Pause in silence (try counting to 10).
- If the patient has not responded after you pause, offer some time alone.→ “Would you like a few minutes alone or would you like me to stay here with you?”
- Seek understanding, and pay attention to patient’s verbal and nonverbal responses.
- Ask open-ended questions.
- If they have not already indicated their feelings, ask an open-ended question.
→ “What thoughts or feelings are coming up for you right now?” - Reflect back.
- If you are not sure if you have understood the patient, reflect back your understanding to check if it is correct.→ “What I’m hearing is that you have a lot of different feelings about finding out that you are pregnant. Am I right about that?”
- Keep in mind that not all patients will feel comfortable disclosing their true feelings.
- Validate and normalize.
- Validate and normalize the patient’s response by expressing understanding.
- Communicate that it is okay for them to feel the way they do.→ “It’s okay not to be happy about a pregnancy/have multiple feelings about a pregnancy. It’s normal to experience and go through several emotions as you are processing this information.”
- Offer to share pregnancy options.
- Offer the patient an opportunity to hear about options in a way that communicates your willingness to discuss all options without judgment.
→“Let me know how I can be most helpful to you. We can discuss any options you are interested in hearing about, including options for ending or continuing your pregnancy, or you can take time to think things over on your own. Either way, you don’t have to make a decision today.” - If they do not want to discuss options at this time, offer written information on all options for patients to read on their own (e.g. Provide Pregnancy Options Flyer).
- Offer the patient an opportunity to hear about options in a way that communicates your willingness to discuss all options without judgment.
Name all pregnancy options.
- Name all pregnancy options (except those the patient expressed they do not want to discuss) in a neutral, professional manner.
→ “If you do not want to continue the pregnancy, I can provide you with referrals for abortion services. If you want to continue the pregnancy, I can provide you with referrals for prenatal care or adoption resources. If you are not sure, we can discuss all of the options available as well as the timeline for abortion options.” Naming each service without bias or judgment respects patient autonomy, builds trust, makes space to ask honest questions and self advocate, and is more likely to meet patient needs.
If the patient is...
Interested in ending the pregnancy
- Visit AbortionFinder.org to find accurate information on limits around gestational age and laws in your area.
- Do not refer to crisis pregnancy centers.
Begin by:
- Mirroring patient language (ex.: “end the pregnancy” vs. “abortion” or “baby” vs. fetus/pregnancy
Screen patient for needs around referral or resources:
- Medication vs. procedural abortion cost and financial aid options (National Network of Abortion Funds)
- Access to services (e.g., language, transportation)
- Parental consent or notification requirements and judicial bypass options (for patients <18 years)
- Addiction treatment, HIV/STI screening and/or treatment, intimate partner violence or survivor support
Offer referral to abortion provider that meets patient’s needs:
- If possible, provide referrals in a written form with the name, address, and phone number of the provider.
- Use AbortionFinder.org to help identify clinics and other supports most accessible to the patient.
- If patient has questions about the procedure, offer to call an abortion clinic with them.
Offer follow up:
- If patient agrees, follow up to review referrals, and offer for them to reach out with questions.
Unsure about continuing or ending the pregnancy
- Gestational age will affect the time they have to make a decision. Visit AbortionFinder.org to find accurate information on limits around gestational age and laws in your area.
- Do not refer to crisis pregnancy centers.
Begin by:
- Offering to answer any questions the patient may have related to pregnancy or abortion
Discuss all options with patient:
- If patient is willing to discuss their feelings, ask open-ended questions in a non-directive manner.
- Allow patient to lead conversation as much as possible.
- If patient wishes, consider the pros and cons of each choice, both in the short and long term.
- Discuss pros and cons in a neutral way, directed by patient concerns.
- Provide information for what medications, drugs/alcohol, and other environmental exposures may be harmful to a developing pregnancy.
- Recommend prenatal care screenings if needed.
- If additional decision support is needed, refer only to providers who approach patients with full respect for any decision they make (All Options Talkline), 1-888-493-0092).
- If patient comes to a decision, reassure and encourage them to trust themselves and their choice. Feelings of shame, disappointment, guilt or regret are normal regardless of the decision.
Interested in continuing their pregnancy
Begin by:
- Affirming the patients decision or interest
- Offering appropriate prenatal care referrals and healthcare provider type preference
- Not referring to services the patient is uninterested in
Screen patient for needs around referral or resources:
- Nutrition, food, and housing security
- Financial resources for prenatal care and/or parenting (presumptive eligibility for Medicaid, WIC, SNAP)
- Overcoming barriers to prenatal care, including transportation, childcare, or translation
- Addiction treatment, HIV/STI screening and/or treatment, intimate partner violence or survivor support
- Early screening for fetal genetic anomalies
- Support for parenting decisions including infant care, adoption, or foster care
- Doula services
- Childbirth education classes or resources
Offer follow up:
- If patient agrees, follow up to review referrals and support resources.
Interested in parenting
Begin by:
- Affirming the patient’s decision or interest
Screen patient for needs around resources:
- Community support (new parent groups, lactation support, trauma and healing support groups)
- Childcare resources
- Financial support available to parents
- Child development education classes or resources
- Prenatal care
Interested in adoption
Begin by:
- Affirming the patient’s decision or interest
- Using affirming language: “planning an adoption” instead of “giving up your baby for adoption;” “birth parent/first parent or “adoptive mother/parent” instead of “real mother/parent”
Counsel patient and provide resources:
- Discuss types of adoption (open, closed, familial)
- Decision support: they can take as much time as needed to decide, and can change their decision up until the time of adoption
Refer and schedule appointments:
- Schedule a visit if your agency provides adoption services. If not, use your agency-approved list of adoption services (i.e., All-Options Adoption Agency or National Pro-Choice Adoption Collaborative).
- If patient is ready, connect them with legal help for reviewing documents and contracts (legal aid, bar association pro bono list).
- Invite patient to follow up as needed.
- Refer to or schedule prenatal care.