Navigating an unintended pregnancy can be a challenge for anyone, but for people with higher body weights, the journey often comes with additional hurdles due to anti-fat bias. Addressing this bias is essential for ensuring everyone receives the quality care they deserve. Let’s dive into how to recognize anti-fat bias, combat it, and create a supportive environment for the people you serve.
Recognizing Anti-Fat Bias
To understand how providers have been affected by the Dobbs decision, we surveyed them about their experiences and learned some important things.
Anti-fat bias is rooted in anti-Black racism and intersects with other forms of oppression such as transphobia, homophobia, classism, and ableism. Anti-fat bias in healthcare can manifest in several ways, often leading to negative experiences and outcomes for patients. Here are some common examples:
- Diagnostic Overshadowing: Imagine going to the doctor for a sore throat and being told to lose weight. Diagnostic overshadowing stems from cognitive bias and occurs when the symptoms of one illness are misattributed to an already diagnosed condition. When healthcare providers attribute all health issues to a patient’s weight, they might miss or delay diagnosing conditions unrelated to weight. For example, menstrual irregularities, fertility problems, or pelvic pain might be dismissed as simply due to higher body weight rather than investigated for underlying conditions like polycystic ovary syndrome (PCOS) or endometriosis. This can lead to inadequate or delayed treatment, compromising patient safety and well-being.
- Disrespectful Behavior: Sometimes, it’s not what is said but how it’s said. Stigmatizing language, negative body language, or dismissive attitudes make patients feel humiliated or disrespected. This behavior can discourage patients from seeking care, being honest about their health concerns, or following medical advice.
- Inadequate Facilities: Ever struggled to fit into a waiting room chair at a doctor’s office? A lack of appropriately sized medical equipment, such as exam tables and blood pressure cuffs, can make visits physically uncomfortable and emotionally distressing. This can further deter people from seeking necessary care.
- Stereotyping: An alarming number of providers report that they perceive fat patients as lazy, unattractive, non-compliant, and unhealthy. Assuming a patient’s weight is solely due to poor lifestyle choices overlooks factors like genetics, medication side effects, or socioeconomic status. These assumptions can lead to biased medical advice and a lack of personalized care plans.
- Differential Treatment: Patients with higher body weights often receive different levels of care or fewer treatment options based on their weight. This can result in substandard care and worsen health disparities.
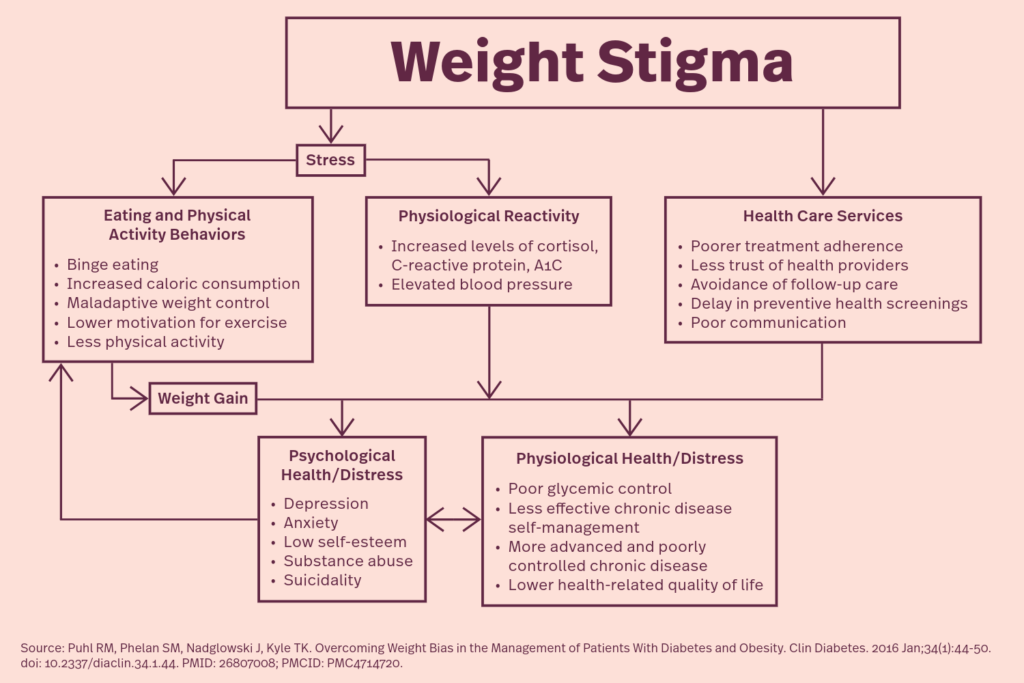
Health consequences resulting from experiences of weight stigma
Anti-fat bias is particularly concerning in reproductive health, where it can manifest in numerous detrimental ways, often resulting in limited access to contraceptives, inadequate prenatal care, and unjust barriers to abortion care.
- Access to Contraceptives
- Misconceptions often lead providers to restrict options without considering autonomy and individual needs and preferences. Assumptions that certain contraceptive methods are less effective or riskier for patients with higher body weights are incorrect. While some studies suggest that certain emergency contraceptives might have reduced effectiveness in patients who weight 165 pounds or more, and possibly no effectiveness for those who weigh 176 pounds or more, this doesn’t necessarily apply to all forms of hormonal birth control. Combination birth control pills, which use both estrogen and progestin, were once thought to be less effective for those with higher BMIs. However, a review of studies showed that there isn’t a clear relationship between a person’s weight and the effectiveness of hormonal birth control. Unfounded concerns about insertion difficulties or complications can lead to hesitation to offer long-acting reversible contraceptives (LARCs) like IUDs or implants, even though people with higher BMIs are more likely to use LARCs than hormonal contraception.
- Contraceptive counseling may disproportionately emphasize weight loss before addressing contraceptive needs, delaying access and increasing the risk of unintended pregnancy.
- Prenatal Care
- Diagnostic overshadowing can lead to missed or delayed diagnoses of conditions that could impact pregnancy. For example, a pregnant patient with higher body weight experiencing symptoms like shortness of breath or fatigue might be advised to lose weight, rather than being evaluated for conditions like anemia or gestational diabetes.
- Stigmatizing attitudes that emphasize weight loss or blame weight for any complications during pregnancy create a negative and shaming environment that can discourage patients from seeking necessary prenatal care.
- Pregnant patients with higher body weights might be referred to high-risk clinics unnecessarily or face limitations on the types of care they can receive based solely on their weight, rather than their overall health condition.
- Many healthcare settings aren’t equipped to accommodate patients of all sizes comfortably. Standard exam tables, blood pressure cuffs, and other medical equipment may be too small or uncomfortable, leading to inadequate physical exams and monitoring. This can affect the quality of prenatal care and increase patient discomfort.
- Abortion Care
- Patients with higher body weights may face delays or outright denials when seeking abortion care. They may be required to lose weight before undergoing the procedure, even when it’s not medically necessary. Because abortion care already requires considerable time restraints, losing weight before the procedure is unrealistic and impossible to do in a healthy way.
- Some clinics have weight restrictions for procedural abortions, forcing patients to seek care at specialized facilities, which may not be readily accessible, increasing travel times, costs, and delays.
- Overestimation of risks associated with abortion care for fat patients can lead to unnecessary caution or refusal to perform certain procedures, despite evidence that higher body weight isn’t associated with increased risk of surgical complications. Overemphasis on potential risks can result in undue anxiety and limited care options.
- Assumptions that medication abortion is less effective or riskier for patients with higher body weights can cause reluctance to prescribe this option, despite evidence that medication abortion is safe and effective across a wide range of body sizes.
- Standard clinic furniture and equipment may not accommodate fat patients, which can make procedures uncomfortable and logistically challenging.
Combatting Anti-Fat Bias
Combatting anti-fat bias is crucial for several important reasons:
- Health and Safety: When it comes to health, everyone deserves a comprehensive evaluation. Eliminating anti-fat bias ensures that every patient receives a thorough and accurate health assessment, which is essential for patient safety. Personalized care that considers individual needs rather than making assumptions about weight can significantly improve health outcomes.
- Trust and Communication: Open, honest communication is the cornerstone of effective healthcare, especially during pregnancy counseling. When patients feel respected and understood, they’re more likely to share pertinent information about their health, lifestyle, and concerns. This open dialogue builds trust between patients and providers, ensuring that guidance and support are truly effective.
- Mental and Emotional Well-being: Experiencing stigma and discrimination can cause significant stress and anxiety. A supportive, bias-free environment helps reduce this emotional burden. Respectful counseling not only empowers patients but also boosts their confidence in making informed decisions about their pregnancy.
- Improved Health Outcomes: Focusing on overall health and well-being rather than just weight allows providers to develop more comprehensive care plans. When patients receive unbiased information and support, they’re better equipped to make informed decisions, resulting in more positive experiences and outcomes.
- Inclusivity and Respect: Everyone deserves to feel valued and supported in their healthcare journey. Ensuring that all patients receive respectful and dignified care, regardless of their size, promotes inclusivity. Combatting anti-fat bias helps address broader health disparities, contributing to more equitable health outcomes.
- Continued Engagement: Positive experiences with providers encourage patients to continue seeking care. Continuous engagement with healthcare and social services is essential for monitoring and maintaining sexual and reproductive health. By creating a welcoming environment, we can ensure that patients feel comfortable returning for care whenever they need it.
Creating a Supportive Environment
Here are some ways you can combat anti-fat bias and create a more respectful and supportive environment for the people you serve:
- Training and Education: Health and social service providers should receive ongoing training on recognizing and addressing anti-fat bias. Increasing awareness and understanding of this issue helps create a more inclusive and respectful environment for all patients.
- Person-Centered Counseling: Focus on individual needs and circumstances rather than making assumptions based on body weight. Counseling should be respectful, empathetic, and nonjudgmental, helping to build trust and ensure patients feel heard.
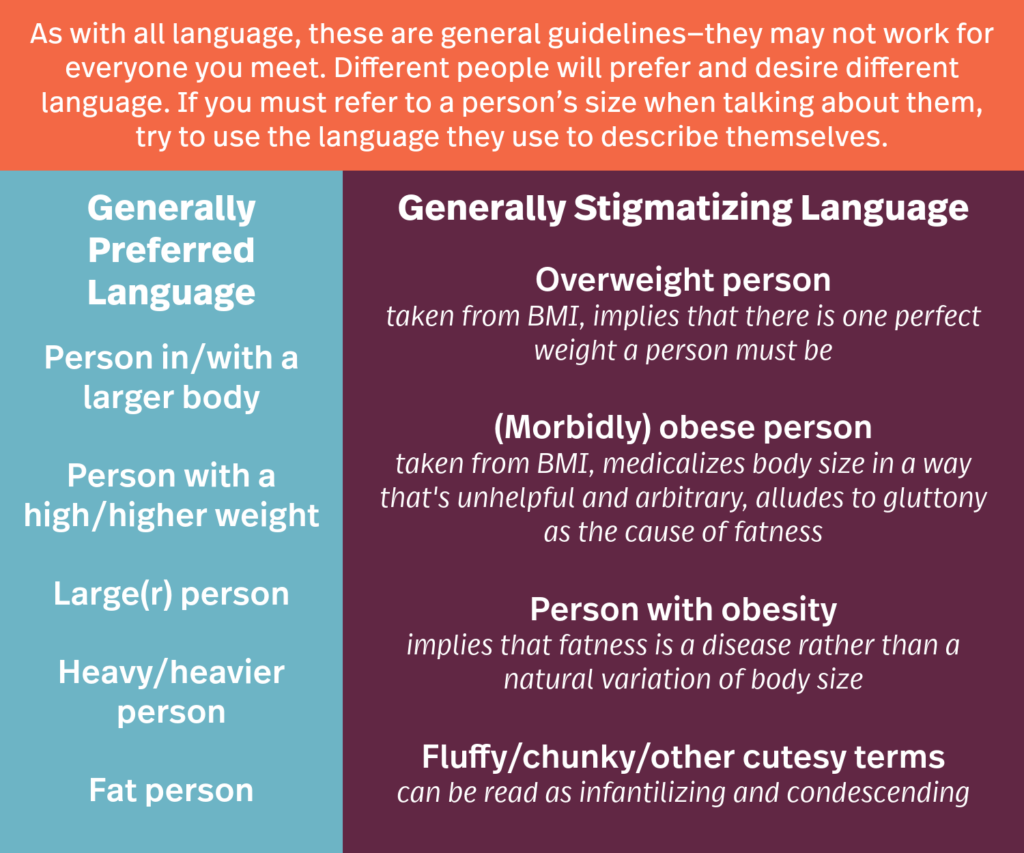
- Inclusive Language: Use neutral and inclusive language when discussing weight. Avoid stigmatizing terms and focus on overall health and wellbeing, which can reduce feelings of shame and stigma and encourage open communication.
- Holistic Approach: Consider all aspects of a patient’s health, including mental, emotional, and social factors, rather than focusing solely on weight. A holistic approach leads to more comprehensive and effective care plans.
- Accessible Environment: Ensure the environment is welcoming and accessible for patients of all sizes. Having appropriately sized furniture and medical equipment creates a more comfortable and dignified experience.
- Patient Advocacy: Provide resources and support for patients to advocate for themselves and navigate healthcare systems. Support groups, educational materials, and counseling services can empower patients and improve their healthcare experience.
-
- The Association for Size Diversity and Health has a directory of providers who use a Health at Every Size® approach in their practice, across all specialties. This approach centers weight inclusivity, health enhancement, respectful care, life-enhancing movement, and eating for well-being.
By recognizing and combatting anti-fat bias and creating supportive environments, you can ensure that everyone receives the care and respect they deserve, regardless of their size. Together, we can create a healthcare system where every individual feels valued and supported.