“As professionals we get caught up in the daily motions. It’s easy just to come into your office and do what you do every day. We lose our genuine effectiveness in helping our patients, and we don’t necessarily stop and examine if we have biases or prejudgment, we don’t think about that when we are just going through the motions. So now when I am meeting with people I am really stepping aside and asking, ‘Am I feeling a certain way, anything that is going to hinder me from helping this patient?’”
Social Services Program Manager, Tennessee
At Provide, our central driving value is the belief in the fundamental and inherent worth of all people—including those who cause us discomfort. Often, this discomfort is a product of stigma: the negative view we hold of people because of a certain quality or circumstance. Stigma sits at the forefront of our work in providing abortion referrals trainings, as well as in the work of many of our partner sites, which includes domestic and sexual violence, family planning, HIV, and substance use disorder. Only by recognizing and working against stigma can we create systems that can truly provide patient-centered care for our clients. Our blog series on stigma discusses how it shows up in health care and social service delivery; how to identify signs and symptoms of stigma at the individual, environmental, and structural levels; and how individuals can help to remove stigma from their workplace.
How to Identify Signs and Symptoms of Environmental Stigma
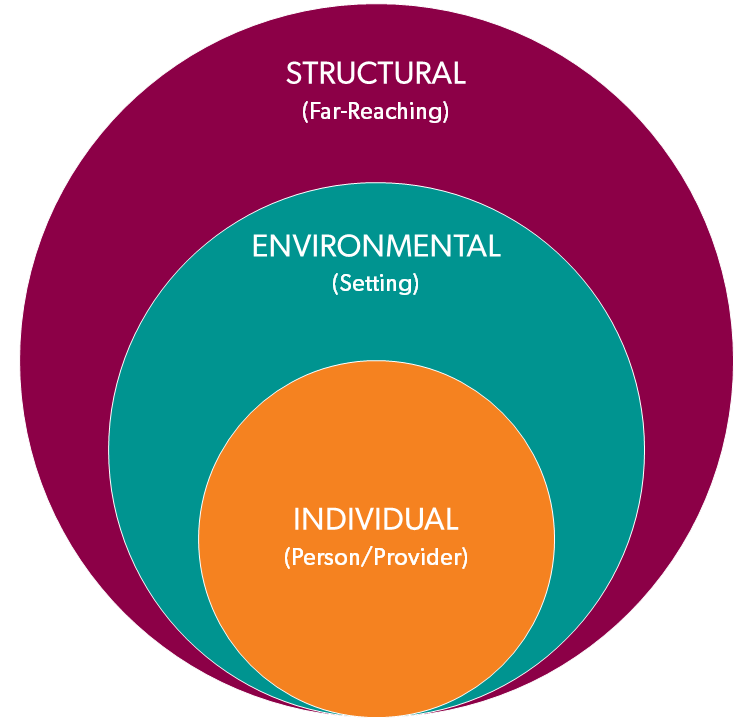
In seeking to identify where stigma might be present in your professional setting, it can be helpful to think about stigma as occurring at three levels:
Individual: from the individual provider who is interacting with the patient/client
Environmental: from the immediate environment where health care and social services are delivered (the community or clinic in which you practice is also part of the environment)
Structural: from the immediate policies and procedures that guide how health care and social services are delivered (this can include individual organizations, as well as local, state, and federal laws and policies)
These levels are interconnected. Individuals can influence their environment to be stigma-free, but structural change requires leadership buy-in. Environmental stigma is important to understand because institutional cultures that normalize stigmatization create social pressure for the health care staff to stigmatize particular patient populations. This may cause a patient to receive sub-par or incomplete care that doesn’t address their needs, and also can influence the provider’s practice throughout their career.
For example, environmental stigma is often attached to people who use drugs. The opening of a methadone clinic in a community is often met with protest, despite the fact that treating substance use disorder with methadone is an effective and evidence-based practice. Methadone treatment itself is also extremely stigmatized. Presumptions are made about substance users and what their presence might mean to a community, which in turn might contribute to a lack of treatment options for those who seek help.
“I think that in this area there is a stigma with substance abuse. Since that’s an area I work with, people are already so afraid to talk about their substance abuse and they minimize it anyways. And if a woman is pregnant and is also using substances, there is even more pressure on her. And, from what I have heard from women, they feel like they’re letting people down, letting their child down. Addiction is addiction. So for me it is just breaking down that wall and talking about it. And the more you talk about it, the more it goes away. It’s kind of like suicide. Just because you don’t talk about it, doesn’t mean it doesn’t exist. The opposite is true. The more you address it, the less it is likely to happen.”
Substance Use Case Manager, Kentucky
Our Referrals Training and Technical Assistance Program attempts to address stigma by reviewing interactions with clients (Individual), staff policies and procedures (Environmental), and leadership initiatives (Structural) that can ensure that people receive the care they deserve without being stigmatized.
“What sticks in my mind, we had a client who was pregnant and she was going to raise the baby. But one day she had someone fax adoption papers, and she never talked to us about it. That always stood out to me. I felt we had failed her, and I wondered, where is the disconnect?”
Domestic Violence Therapist, South Carolina
Visual cues can signify to clients whether they might be stigmatized at a clinic and can also informally signify to staff what may be acceptable or unacceptable practices in the workplace. For example, placing a bowl of condoms out can signify to clients that they can talk about safe sex. Having pregnancy posters or brochures that discuss all three pregnancy options (parenting, adoption, and termination) in bathrooms and waiting areas signifies that patients can be comfortable talking about current or past reproductive health history. Some questions to ask to help you determine whether environmental stigma exists in your workplace include:
- Do your policies, programs, and practices perpetuate or tolerate discriminatory behaviors?
- Is there limited access to evidence-based information and training for clients and staff?
- Do you serve LGBTQIA+ clients? How does your community know?
- What visual cues are present that signify to clients and staff that your workplace is warm, welcoming, non-judgmental, and inclusive of all people? Are there any visual cues that may signify judgment of particular choices?
- Does your workplace have harm reduction policies, programs, and practices?
- Are Patients’ Rights visible and accessible?
WHEEL OF CHANGE
The Wheel of Change is a model for transformation: change that is profound and fundamental, altering the very nature of something. Transformational change is both radical and sustainable.
- Heart & Mind: The full range of what people think and feel—motivations, beliefs, emotions, perceptions, etc.
- Behavior: What human beings do—our words and deeds, the actual choices we make to speak or not speak, to act or not to act.
- Structures: The external environmental realities which impact Hearts & Minds and Behavior—the micro systems and structures that make up our individual lives: the organizational systems, structures, and processes in which we work, and the larger social and economic systems that dominate our society.
The behavior of those within an organization or environment is driven by what they think and feel (Heart & Mind), while also being influenced by the organizational Structures in which they work. Peoples’ thoughts and feelings (Heart & Mind) are strongly influenced by the Structures in which they work, while also being impacted by the Behavior of those around them. The collective Heart & Mind and Behavior of staff, in turn, contribute to shaping and reshaping organizational Structures.
For more resources on addressing environmental stigma, visit Tools for Transformation – WHEEL OF CHANGE: A Model for Personal Transformation By Robert Gass.
Identifying the personal and institutional biases that exist is an important step in addressing environmental stigma. Before we’re able to address environmental stigma and change can happen, it’s critical to acknowledge that the transformation we seek is one piece of a larger organizational system, and that it is interconnected and interdependent with other parts of the system. By engaging in this systemic approach, we can create a cycle in which changes in one sphere incite and reinforce change in the other two domains for the benefit of workers and the people they serve.
How can you address environmental level stigma in your workplace?
- Review patient-facing materials such as pamphlets or flyers for stigmatizing language and revise as needed.
- Include visuals (posters, infographics, etc.) in your lobby and exam rooms that are inclusive of patients from a multitude of backgrounds and experiences.
- Communicate on your website that your services are patient-led and provide referrals to resources that honor patients’ autonomy.
More quotes about stigma from providers who have attended our Referrals Training:
Going to [Provide’s] training helped me understand that I needed to slow down, listen, and be more empathetic and understanding. We have about 15 minutes with each client; we are rushed. And I think more than anything else that the training helped me understand how important it is to give her time, and let her process as much as she can within the limited time we have in clinic, and to give her all the options she has in an unbiased manner. When I was rushed before, I would just say, ‘This is what you’ve got, here you go.’ But after, I would take the time to make eye contact and really consider this person in front of me. She’s not a number, she’s got a life-altering decision to make, and she is at a crossroads. And trying to quiet my thoughts about speed and other patients, to sit there and connect with that person. That was brought home in the class. Give her the respect she deserves, and the honesty and time she deserves in the time you have. Make that visit as personal as…make her feel like she has an advocate for her. And I learned to say after each visit, ‘Remember, if you need me, call me.’ To make sure she knows there is someone she can talk to later on when this thing starts hitting her even more deeply than it did today, she can call back. I began to say, ‘You can call me if there’s anything I can do, even if you just want to talk.’ To let her know she had a friend who would listen to her. I just started to look at her more as a person than a patient, and offering to help her later if we can, to give her birth control if she chooses to let us help her. Or to talk with her if she has questions about the pregnancy.
Nurse, South Carolina
“When we are working with any specific community and women look for orientation and support I now pay attention and try to be open, and most of all, to talk naturally about this information. To normalize it. Sometimes is so difficult for Latino communities, even to ask for condoms. We have a place full of condoms here and sometimes since it is a taboo, women just don’t ask for them. Sometimes it is so simple but yet so difficult. Now I try to talk more naturally about reproductive health issues. I don’t know, differently, trying to show women that we won’t think they are doing something wrong, without judging them.”
Health Program Director, North Carolina
Previous: How to Identify Signs and Symptoms of Individual Stigma
Next: How to Identify Signs and Symptoms of Structural Stigma

